The federal Centers for Medicare and Medicaid Services (CMS) Interoperability at its core aims to ensure all participants have access to standardized data. The overall concept is fundamentally built on the idea of a “golden record,” a unified master directory of provider information. This is where a Master Data Management platform with matching capabilities can relieve the resource burdens to meet the requirements.
The 21st Century Cures Act aims to “implement provisions that will advance interoperability and support the access, exchange, and use of electronic health information” and includes requirements from the Office of the National Coordinator for Health Information Technology (ONC). The three-part requirements introduce the use of Faster Healthcare Interoperability Resources (FHIR) to advance healthcare in delivering data via standardized formats.
The first of the requirements is Patient Application Program Interface (API) which must be available to third-party providers to develop web and mobile applications by January 1, 2021. Penalties from CMS began on July 1, 2021.
While FHIR is a required standard for delivery of the data, there are several recommendations for methods by which to implement those standards.
Regardless of the FHIR standard selected for implementation, the key challenge is acquiring, developing, matching, and managing the data associated with many sources of record. It is a misstep to believe the Electronic Health Record (EHR) will exclusively meet the requirements of each CMS requirement related to Interoperability.
How does Master Data Management (MDM) help?
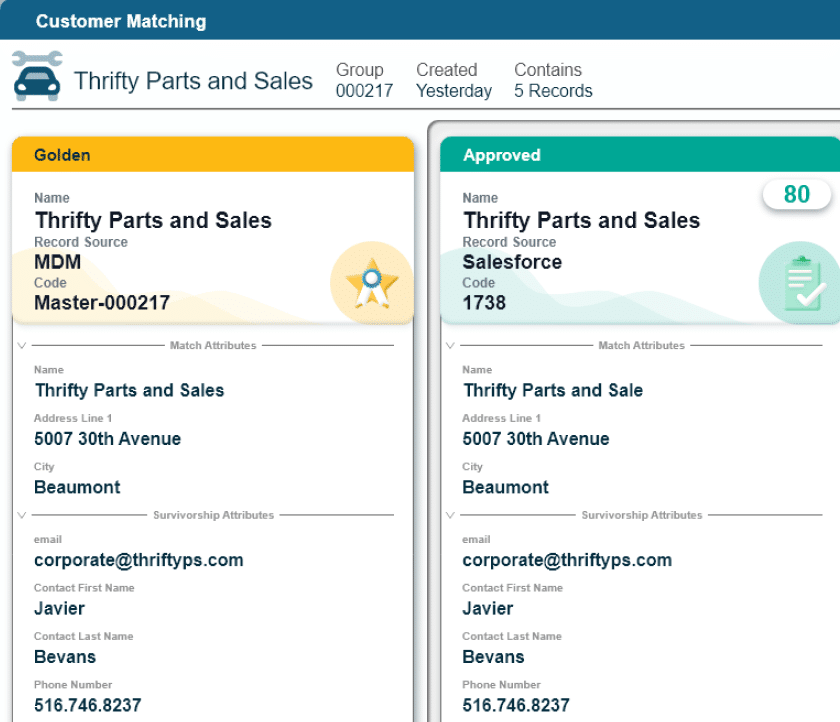
MDM is a critical component of the overall Interoperability requirements due to the management of many data sources with common types of data. While the objective is to produce a single record for each patient, provider, claims transactions and more, the ability to produce unique “master” records is dependent on having the right technology in place.
Master Data, as a principle, is designed to match records from multiple data sources to identify data quality variations and to engage subject matter experts or Data Stewards who can then review and/ or correct errors.
Using workflows and automation via an MDM platform like Profisee allows the business to participate in workflows that provide timely updates, improve, and then maintain the quality of the data that is then used across multiple enterprise-wide platforms. While CMS Interoperability requirements are so significant that having an MDM platform is a requirement, the use cases span far beyond CMS Interoperability
Provider Data
Master Data streamlines processes and reduces the overhead of manual lengthy mapping and matching processes that take weeks to months to resolve over and over throughout a calendar year.
The following is one scenario applicable to provider data. Many healthcare organizations and providers are choosing to use the Fast Healthcare Interoperability Resources (FHIR) Standard called “Da Vinci” to develop the necessary mappings for the second phase of CMS Interoperability requirements, better known as the Provider Directory Application Programming Interface (API).
Regardless of the FHIR standard, the CMS Implementation guides indicate that Provider Demographic values must be standardized according to the National Uniform Claims Committee (NUCC) requirements for provider taxonomy and associated descriptions.
While many upstream data sources, such as Provider Credentialing Systems, manage their data according to the NUCC Taxonomies, they do not all abide by the Taxonomy Description values. The more common practice is to customize or modify the taxonomy descriptions based on what the local practice and/or the provider’s electronic health records system prefer to display.
Without Master Data Management (MDM) technology developers would need to create crosswalks from each source, obtain approvals from the business lines subject matter experts, and then map them to the NUCC Taxonomy to meet just one of the Provider Directory API standards.
The additional effort would be required to safeguard that the specialties are not mapped to the provider’s board certifications (this is especially important for all clinicians who are not Medical Doctors or Doctors of Osteopathy who do not have general board certifications and/or are not required to have board certifications).
To manage the process described above would require environments, workflows, and cumbersome manual processes repeated continuously throughout the year. With Master Data Management (MDM) technology this process is developed once and set-up via automatic updates to reference tables. Data stewards can then update new tables when they are available from the NUCC data source and update mappings when automated notifications are sent to them as prompted by new values.
Patient Data
The Federal Register containing the requirements and recommendations for the management of patient data includes the following: “We encourage the use of standardized elements to accurately represent patient addresses including the use of standardized references in the
U.S. Postal Addressing Standards where applicable. In addition, we will continue to work with standards developing solutions to improve patient matching… including formats for health IT use cases.”
Master Data Management technologies solve each of the requirements and offer integrations to U.S. Postal Standards and even more location identifiers such as Geospatial Data. It also helps healthcare organizations deliver standardized address values for patients, manage the mappings, the continual updates and changes, the multiple types of addresses, the data quality variances, and the stewardship of issues resolution.
Reference Data
Each of the CMS Interoperability Phases requires substantial use of standardized sets of reference data. The value sets are made up of one to many code sets, code values, and associated standards. Many of the FHIR Standards for suggested implementation require the use of external reference data sources via code sets that are licensed (e.g. American Medical Association (AMA) codes).
Furthermore, internal standards (or those mandated by CMS) must be developed to crosswalk values from data sources to the normalized output before sending data to third-party vendors, payers, and CMS.
For each of the above scenarios the management of and enforcement of reference data is best facilitated through Master Data Management (MDM) Platforms. Check out the core capabilities of the Profisee MDM platform here.
To successfully meet the requirements of CMS Interoperability, Master Data is the source data that offers the underpinnings of a successful product. It ensures high quality and standardized data is sent to third-party vendors and subsequently seen by members and patients. Master Data enables an organization to stand behind the data they produce that will soon be very publicly committed via Payers, Patients, Provider, and CMS.
Click here for more information on how Profisee is supporting clients with Master Data Management Technologies to streamline their Data Management processes.

Forrest Brown
Forrest Brown is the Content Marketing Manager at Profisee and has been writing about B2B tech for eight years, spanning software categories like project management, enterprise resource planning (ERP) and now master data management (MDM). When he's not at work, Forrest enjoys playing music, writing and exploring the Atlanta food scene.