Leading Non-Profit Healthcare System Accelerates Eligibility and Prior Authorization with Profisee
Using MDM to unify fragmented patient and payer data for faster, more accurate authorization decisions
reduction in erroneous matches
increase in claims processing throughput
Industry: Healthcare
Customer: Since 2019
Data Types Mastered with Profisee
- Patient data
- Payer data
This leading non-profit healthcare system operates hundreds of care locations across multiple states, spanning primary, urgent, pediatric and specialty care centers, as well as a robust network of hospitals. The organization is committed to delivering compassionate care, supporting at-risk populations and improving community health outcomes at scale. It is recognized as one of the largest community-based health systems in its region, serving hundreds of thousands of patients each year across inpatient, emergency and ambulatory services.
Serving a large and diverse patient base — including many individuals without private insurance, a primary care provider or a consistent medical history — the healthcare system faced ongoing challenges verifying eligibility for government-funded programs. Frequent changes in residence or insurance coverage made accurate eligibility determination difficult and slowed the prior authorization process.
Submitting compliant authorization requests required extensive, validated data spanning demographics, contact information, coverage details, medical history, diagnoses and services rendered. For transient and vulnerable populations, this information was often incomplete, inconsistent or spread across multiple systems. The result was significant manual effort, delayed submissions and slower care delivery.
After successfully using Profisee MDM to harmonize provider data across the enterprise, the healthcare system expanded its implementation to address eligibility determination and prior authorization challenges.
The organization aimed to automate the consolidation and validation of fragmented patient and payer data, improving efficiency for authorization teams and ensuring submissions were complete on the first attempt. Because government-funded programs require strict compliance and precise documentation, the system needed a dependable way to ensure timely, accurate and compliant submissions.
The Solution
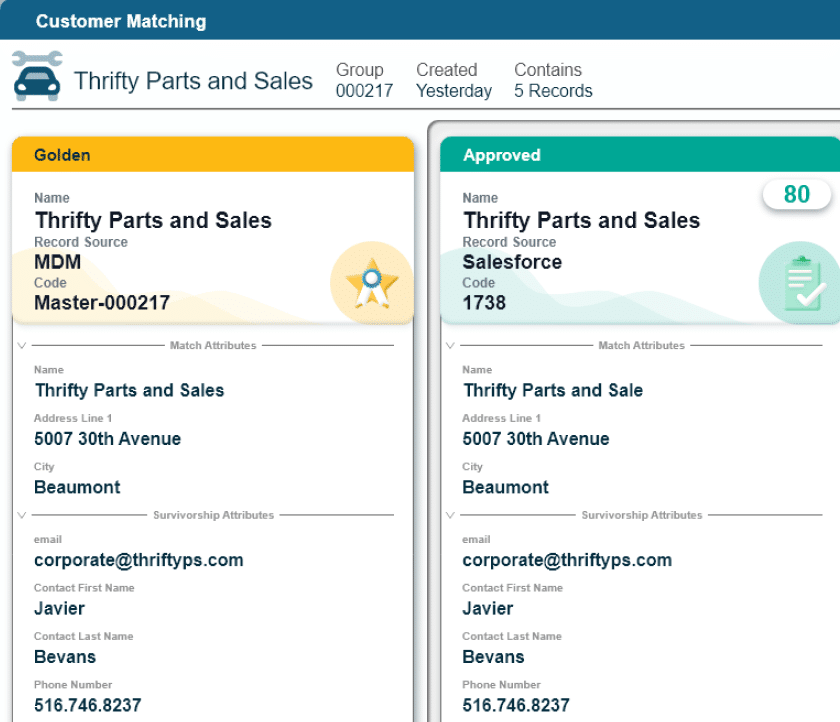
To meet privacy and security requirements, the healthcare system deployed a dedicated Profisee instance to manage patient and member data independently. Using Profisee’s intelligent, multi-step matching capabilities, the team can now accurately link and consolidate records across multiple coverage changes and payer sources.
This curated patient data is combined with electronic medical record (EMR) information to create a comprehensive and unified view. Manual investigations that once consumed significant staff time are now automated, and Profisee’s validation tools flag incomplete or incorrect data before submission. This ensures eligibility and authorization decisions are based on complete, trusted and compliant information.
The Wins
With Profisee, the healthcare system introduced intelligent automation that transformed previously manual, error-prone processes. Earlier attempts to match patient data with SQL or Python scripts were inaccurate and inefficient. Profisee reduced erroneous matches by 60% and saved an average of 5-10 minutes per case, allowing teams to redirect two-thirds of their time to higher-value work.
As a result, each eligibility team member can now process 12-14 claims per hour — a fourfold increase in throughput. These improvements support operational efficiency, reduce administrative costs and ensure accurate, timely and compliant submissions that ultimately enable faster, more effective patient care.
Read additional case studies

Learn how a leading healthcare system streamlines eligibility and prior authorization workflows with Profisee to improve patient outcomes.
Read More
Discover how a leading European public utility used Profisee MDM to unify data, improve billing accuracy and boost operational efficiency.
Read More
Discover how Aker BP uses Profisee and Microsoft Fabric to build a trusted data foundation that powers AI-driven exploration and production.
Read More
Discover how Batory Foods built a modern data platform with Profisee to drive growth and international expansion.
Read More
Discover how WSP Global uses Profisee Master Data Management (MDM) to enable cross-sell growth through a single, trusted client view.
Read More
See how Synovus Financial unified customer and household data with Profisee to uncover cross-sell opportunities and ensure seamless service.
Read More
Learn more about how private commercial real estate finance and investment firm Greystone Financial uses Profisee MDM to overcomes its data challenges.
Read More
Learn more about how AXIS Capital uses Profisee to accelerate core insurance processes, reduce risk and improve management visibility.
Read More
Learn more about how this national healthcare group uses Profisee MDM to improve the patient experience and increase operational efficiency.
Read More
Learn more about how Lexmark uses Profisee to create business-ready data to power its demand forecasting algorithm and boost revenue.
Read More
Learn more about how a specialty insurance carrier uses Profisee MDM to automate and manage its full broker lifecycle and greatly reduce onboarding times.
Read More
Learn more about how Rheem uses Profisee MDM to manage its installer, distributor and retailer data to identify cross- and up-sell opportunities.
Read More
Learn more about how Boyne Resorts uses Profisee MDM to integrate and manage its customer data from disparate systems across its 11 properties.
Read More
Learn more about how YMCA of the USA uses Profisee MDM to integrate, match, merge and standardize its staff data from 763 branch locations across the US.
Read More
Learn more about how Mass General Brigham uses Profisee MDM to let patients find a provider through a provider lookup system.
Read More