Table of Contents
- The Provider Data Problem: A Persistent Challenge
- The Business Impact of Bad Provider Data
- The Provider Hub: How MDM Solves the Challenge
- How Profisee Customers Are Leveraging Provider Hubs Today
- Beyond Providers: The Value of Multidomain MDM
- Conclusion: Modernizing Provider Data Is a Strategic Imperative
- References
Key Takeaways
Fragmented and outdated provider data slows onboarding, causes claim denials and undermines patient trust.
A Provider Data Hub powered by MDM unifies systems into a single, trusted source of truth for provider information.
Healthcare leaders using Profisee’s MDM platform are improving compliance, efficiency and patient experiences across the board.
Before joining Profisee nearly five years ago, I worked in B2B marketing at a large, publicly traded post-acute care provider with more than 500 locations across the U.S. One of the most persistent challenges our operations teams faced was managing provider data from the health systems and acute-care settings we partnered with as patients transitioned from the hospital to recover at home. And the accuracy, timeliness and completeness of their provider data directly influenced our ability to deliver timely, high-quality care.
What struck me then — and what I continue to hear today in conversations with Profisee customers — is how universal this problem is. Whether you’re a home health agency, a hospital or a specialty care practice, the underlying issue is the same: Provider data is constantly changing, yet the systems we rely on to capture and share it are fragmented and inconsistent. Physicians switch networks, earn new credentials and split time across multiple facilities. Data decays and becomes outdated. The result is a messy, incomplete picture that creates inefficiencies and frustration for everyone involved.
Accelerate Microsoft Fabric Success
The Provider Data Problem: A Persistent Challenge
Provider data churn is constant. Doctors move between facilities, gain new certifications, change affiliations or update their practice locations at a staggering pace. IDC Health Insights has estimated that annual churn rates for provider data — including demographics, status changes and affiliations — are in the double digits[ 1 ]. Yet many health systems and health plans attempt to manage these changes with spreadsheets, outdated credentialing systems or manual phone calls. The consequences are predictable:- Inaccurate provider directories that mislead patients and trigger CMS audits[ 2 ].
- Delayed credentialing processes that leave providers waiting weeks or months before they can see patients and generate revenue.
- Duplicate records across systems that create billing errors, mismatched claims and wasted staff hours.
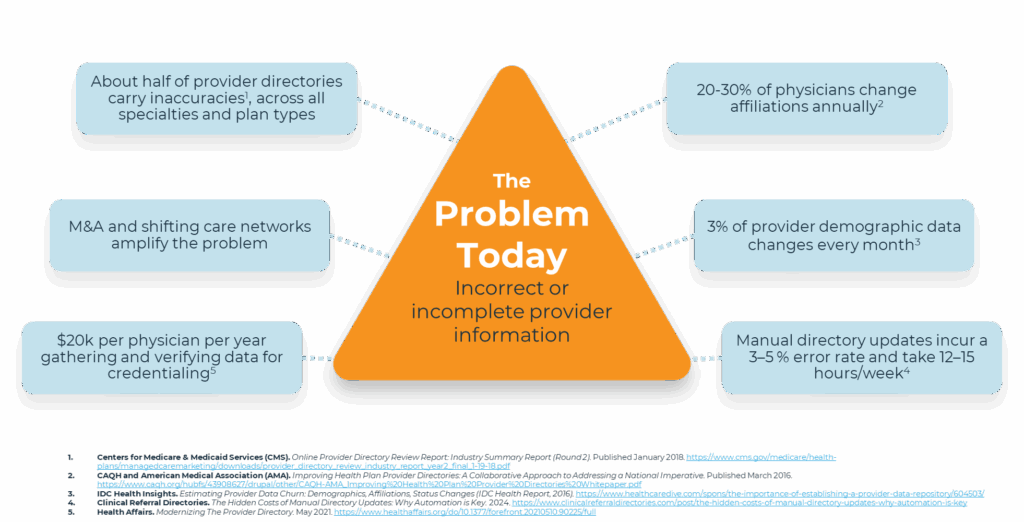
The Business Impact of Bad Provider Data
Poor provider data quality doesn’t just create back-office headaches, it impacts every part of the healthcare organization.
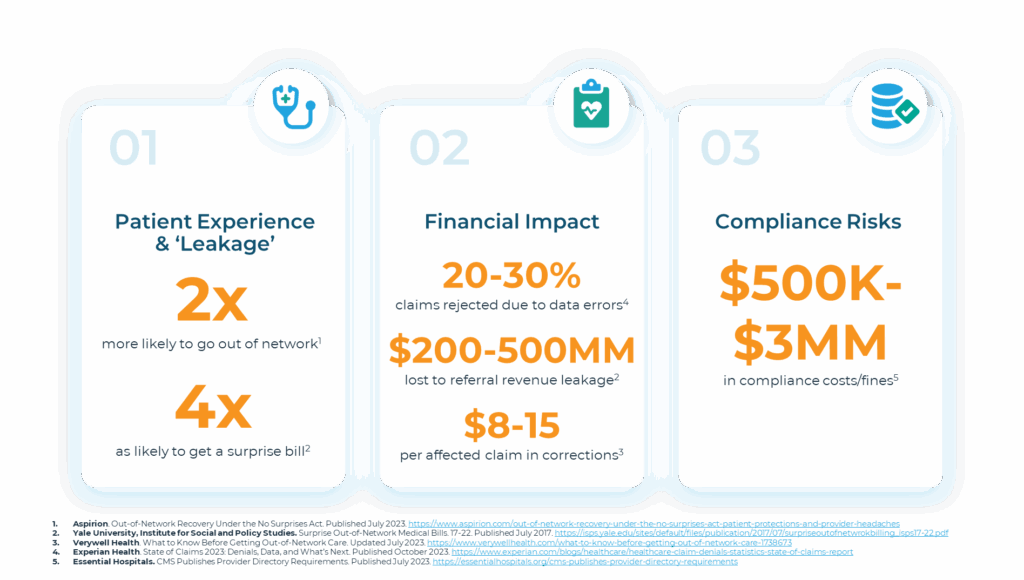
Claims and Prior Authorizations
Inaccurate provider data is one of the leading causes of claim denials. Experian Health’s 2023 State of Claims report noted that denied claims cost healthcare billions annually[ 5 ]. Each denial requires costly rework — or worse, lost revenue altogether.Revenue Leakage
Incorrect referral data leads to patients being directed out of network, eroding revenue potential. Under the No Surprises Act, this also exposes providers to compliance headaches and balance billing disputes[ 6 ].Patient Experience
When patients can’t find the right provider in a directory — or worse, show up to an appointment only to discover outdated information — their trust in both the provider and payer erodes. Health Affairs has argued that modernizing provider directories is essential to restoring patient trust[ 7 ].Learn how Profisee helps organizations optimize scheduling and patient experience.
Compliance & Risk
With CMS enforcing stricter directory requirements, health plans risk penalties and reputational damage if inaccuracies persist[ 8 ].Explore how Profisee enables interoperability and CMS compliance.
The Provider Hub: How MDM Solves the Challenge
So how do you solve a problem as entrenched and wide-ranging as provider data chaos? Enter the provider hub.
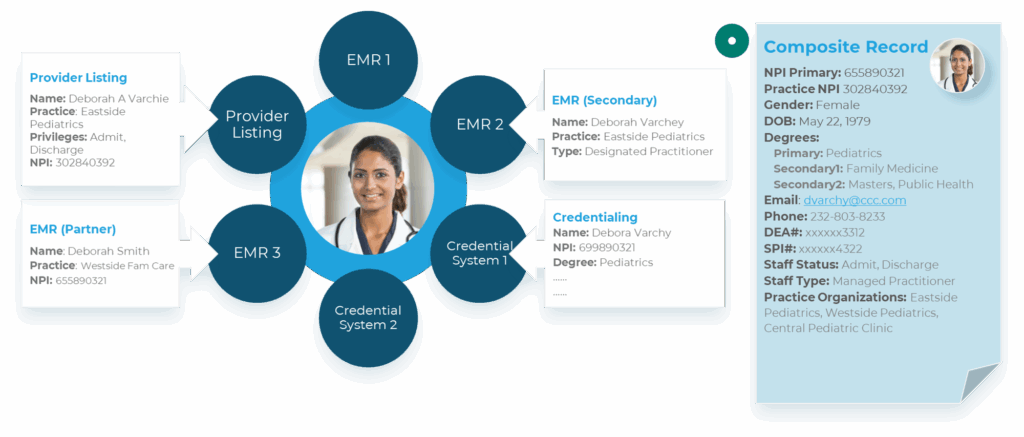
A provider hub built on Profisee MDM unifies provider records across all systems, creating a single source of truth that can be trusted by every department and workflow:
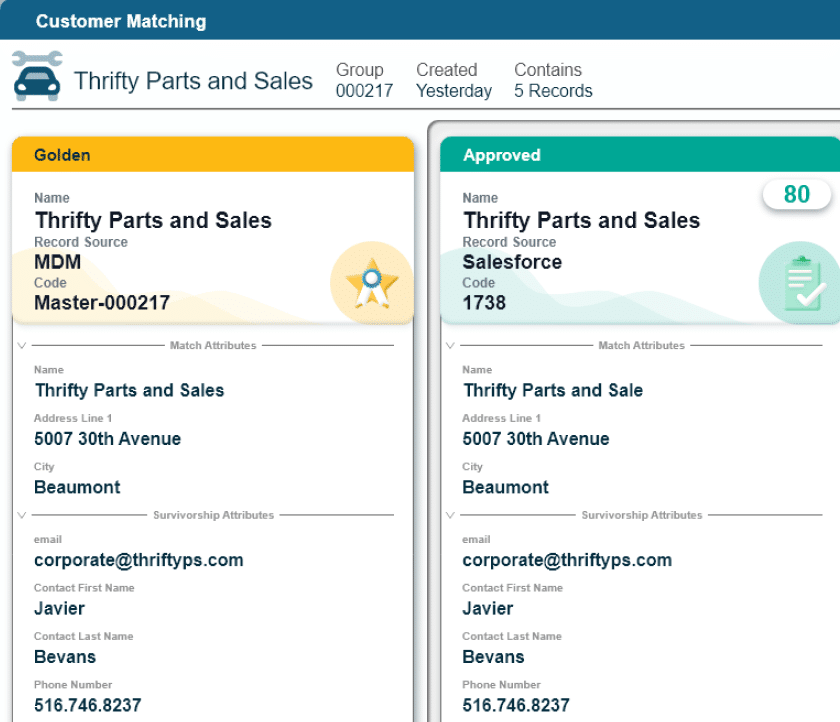
- Entity resolution: Match and merge multiple variations of the same provider (e.g., Deborah Smith vs. Debora Varchy) into a single golden record.
- Data stewardship and governance: Establish clear processes for who owns what data and how updates flow bi-directionally across systems.
- Integration and synchronization: Ensure EMRs, HR systems, directories and claims platforms are all consuming the same trusted data.
With this foundation, healthcare organizations can streamline credentialing, reduce claim denials, improve directory accuracy, and support better patient access.
How Profisee Customers Are Leveraging Provider Hubs Today
Profisee customers are already seeing measurable impact from their provider hub implementations.Mass General Brigham
Mass General Brigham — one of the largest integrated health systems in the U.S. — turned to Profisee to tackle its complex provider data challenge. With over 20 source systems feeding into fragmented provider records, onboarding new providers was slow and error-prone. By implementing a provider hub with Profisee, Mass General Brigham achieved:- 30% less time to onboard new providers
- 20+ source systems matched and merged into a single golden record
Vituity
Vituity, a leading physician-led and owned partnership, faced the challenge of unifying provider data across its vast network to support efficient care delivery. By leveraging Profisee, Vituity built a trusted provider hub that improved data quality, reduced administrative overhead and enhanced collaboration across teams. Their story demonstrates how provider data management is not just about compliance, but also about enabling clinicians to focus on what matters most — delivering high-quality care.Beyond Providers: The Value of Multidomain MDM
So far, I’ve spent most of this blog focused on provider hubs — because they’re often the first and most impactful place to start. But the value of MDM in healthcare extends far beyond just managing provider data. This is where multidomain MDM comes into play. By applying the same principles of unification, governance, and stewardship across other domains, healthcare organizations can solve a wide range of challenges.Member (Patient, Guarantor) Hub
Patient data is often scattered across EHRs, billing systems and intake platforms. A member hub links these records, enabling:- More accurate prior authorizations
- Reduced referral leakage
- Elimination of duplicated administrative work
Asset Hub
Health systems rely on an enormous inventory of medical equipment, devices, and infrastructure. With MDM, organizations can:- Track and manage assets in real time
- Reduce downtime for critical equipment
- Avoid over-purchasing or underutilization
Facility/Location Hub
Hospitals often struggle with inconsistent naming conventions across facilities, clinics, rooms or departments. A facility hub provides:- A single source of truth for all sites
- Improved emergency planning and regulatory audits
- Support for facility-based analytics and resource planning
Supplies Hub
Supply chains in healthcare are notoriously complex. By centralizing supplier and product data, health systems can:- Eliminate vendor duplication
- Improve contract compliance
- Optimize purchasing and procurement workflows
Reference Data Management
Finally, MDM helps organizations govern reference data sets, including ICD-10, CPT, SNOMED and internal lists. With consistent terminology across systems, it becomes easier to:- Map external standards to internal variations
- Improve reporting and downstream analytics
- Ensure consistency across clinical and operational workflows
Conclusion: Modernizing Provider Data Is a Strategic Imperative
Healthcare’s provider data problem is not new, but the stakes are higher than ever. Between CMS directory mandates, the financial toll of denied claims and the consumerization of patient experience, the cost of inaction has never been greater. A provider data hub powered by MDM offers a proven, scalable solution. By consolidating fragmented provider data into a single trusted source, healthcare organizations can reduce waste, improve compliance and enhance patient experiences. Just as I saw firsthand in my years in home healthcare, when a hospital record was incomplete or a physician’s credentials weren’t updated, it could delay the handoff of a patient from the hospital to our home health teams. That same challenge is still playing out across the healthcare system today. The difference now is that health systems, payers and provider groups no longer have to accept these inefficiencies as inevitable. With the right data foundation, they can ensure every provider record is accurate, every credentialing process is streamlined, and every care transition — whether between hospitals, specialty clinics or home health agencies — happens seamlessly. That’s the promise of a modern provider data hub, and it’s why so many organizations are turning to Profisee to make it a reality.Next Steps
- Explore our healthcare MDM solutions
- Dive into healthcare-specific use cases
- Download our expert guide on Provider Master Data Management for Healthcare
References
- ^ IDC Health Insights. Estimating Provider Data Churn: Demographics, Affiliations, Status Changes (IDC Health Report, 2016). https://www.healthcaredive.com/spons/the-importance-of-establishing-a-provider-data-repository/604503/
- ^ Centers for Medicare & Medicaid Services (CMS). Online Provider Directory Review Report: Industry Summary Report (Round 2). Published January 2018. https://www.cms.gov/medicare/health-plans/managedcaremarketing/downloads/provider_directory_review_industry_report_year2_final_1-19-18.pdf
- ^ Centers for Medicare & Medicaid Services (CMS). Online Provider Directory Review Report: Industry Summary Report (Round 2). Published January 2018. https://www.cms.gov/medicare/health-plans/managedcaremarketing/downloads/provider_directory_review_industry_report_year2_final_1-19-18.pdf
- ^ CAQH and American Medical Association (AMA). Improving Health Plan Provider Directories: A Collaborative Approach to Addressing a National Imperative. Published March 2016. https://www.caqh.org/hubfs/43908627/drupal/other/CAQH-AMA_Improving%20Health%20Plan%20Provider%20Directories%20Whitepaper.pdf
- ^ Experian Health. State of Claims 2023: Denials, Data, and What’s Next. Published October 2023. https://www.experian.com/blogs/healthcare/healthcare-claim-denials-statistics-state-of-claims-report
- ^ Aspirion. Out-of-Network Recovery Under the No Surprises Act. Published July 2023. https://www.aspirion.com/out-of-network-recovery-under-the-no-surprises-act-patient-protections-and-provider-headaches
- ^ Health Affairs. Modernizing The Provider Directory. May 2021. https://www.healthaffairs.org/do/10.1377/forefront.20210510.90225/full
- ^ Essential Hospitals. CMS Publishes Provider Directory Requirements. Published July 2023. https://essentialhospitals.org/cms-publishes-provider-directory-requirements

Benjamin Bourgeois
Ben Bourgeois is the Head of Product and Customer Marketing at Profisee, where he leads the strategy for market positioning, messaging and go-to-market execution. He oversees a team of senior product marketing leaders responsible for competitive intelligence, analyst relations, sales enablement and product launches. He has experience managing teams across the B2B SaaS, healthcare, global energy and manufacturing industries.