- HEALTHCARE Use Case
STREAMLINE PROVIDER CREDENTIALING
How Profisee can help healthcare organizations streamline and empower their credentialing teams and tools.
Provider Credentialing
Provider credentialing has grown increasingly complex and is often a slow, costly, error prone process. For this reason, specialty software solutions have come into the market to help manage the process. However, for complex healthcare organizations with many facilities and multiple EMR and other core systems, assembling the essential data needed by credentialing solutions is its own challenge.
Data Domains
Provider, CPT & HCPS codes, Location
Business Problem
Delayed revenue cycles, under-utilized staff
Teams Impacted
Operations, HR, Risk, Accounting
MDM Impact
Onboard new providers more quickly
Excess Costs & Delays in Credentialling
- Numerous data sources: Required data comes from multiple internal and external sources and is often incomplete or conflicting.
- Highly manual processes: Typically multiple staff are involved to manually gather and reconcile all data needed for initial and ongoing credentialling.
- Excessive cost: Due to manual processes, it is estimated provider credentialling costs $20,000 or more per year per credentialed provider.
- Underutilized staff: Due to a lengthy manual process, staff and contracted providers are unable to perform billable services until credentialling is complete.
- Delayed revenue cycles: While awaiting the slow and cumbersome credentialing process, billable services are not performed, yet provider costs continue to accrue.
- Provider turnover: Providers get frustrated with delayed revenue and payments and may seek employment elsewhere.
Streamlined, Accurate Data Aggregation
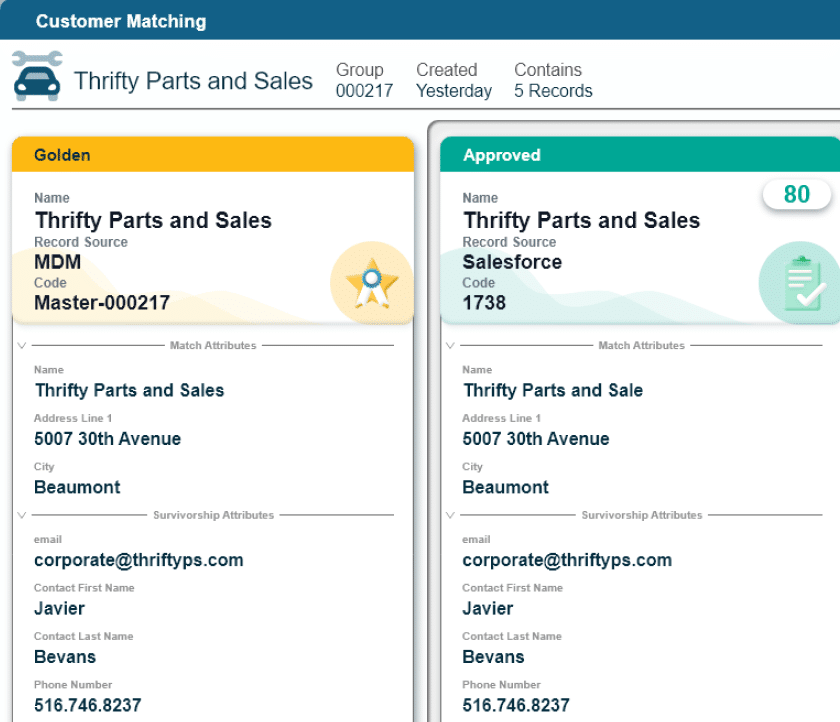
- Single point of data aggregation: With the ability to consolidate data from multiple sources into a single golden provider records, MDM provides a centralized place where data can be automatically merged and then reviewed and remediated by credentialling staff.
- Actionable business rules: Configurable business rules alert credentialling staff of missing or invalid data proactively.
- Automated workflows: Workflows triggered upon staff actions, automated linking and merging, or business rules help accelerate the credentialing process forward with full visibility.
- Get the data right the first time: With data fully assembled and validated, with automated and AI based assistance, credentialling teams and tools get the data they need faster and with fewer errors.
Faster Provider Onboarding & Patient Care
- Reduce time to onboard providers: Get new providers on-boarded and performing billable activities faster.
- Reduce credentialling costs: Much of the cost to credentialling is seeking out missing, inconsistent or invalid data – with MDM, this effort is greatly reduced.
- Reduce service to payment intervals: With more accurate and complete data, the credentialling processes with payers and managed care organizations is faster and more accurate, resulting in faster payments for services provided.
- Reduce disputed payment claims: Payment claims will be delayed if provider credentials are incomplete or out-of-date. With credential data complete and accurate the first time, these errors are prevented.
- Reduce provider turnover: Reduce provider frustration caused by delayed onboarding.