- HEALTHCARE Use Case
Streamline Prior Authorization
How Profisee can bring powerful automation to the process of assembling and validating data required for prior authorizations.
Reduce Errors & Overhead to PA Submissions
With a myriad of policies spanning different plans and payers, prior authorizations are a difficult and time-consuming part of any medical practice. It is estimated that the annual per-physician cost for prior-authorization submission and follow up can be as much as $70,000 per year. A significant portion of the cost and effort associated with prior authorization submissions is manually gathering and validating all the patient, plan, and medical details required. This is where Profisee helps.
Data Domains
Patient, Member, Plan, Reference Data
Business Problem
Excess costs and delays in care associated with PA
Teams Impacted
Operations, Billing, Physicians
MDM Impact
Streamline PA submissions for faster authorization
Excess Costs & Delays with PA’s
- Delays in Treatment: Data errors in PA submissions can lead to submission rejection, requiring manual correction and appeal/resubmission. This ping-pong between providers and payers can result in substantial delays in delivering care.
- Administrative Overhead: For many healthcare organizations, assembling and validating the data for PA submissions is highly manual.
- Excess Denial Rates: Incorrect or incomplete data in PA submissions can result in invalid coverage denials and require sometimes repeated remediation prior to care delivery.
- Physician Burnout: “As a physician, prior authorization is the number one frustrating thing of practicing outpatient medicine right now, far and away” –Dr. Gabriel Bossle, Indianna University School of Medicine
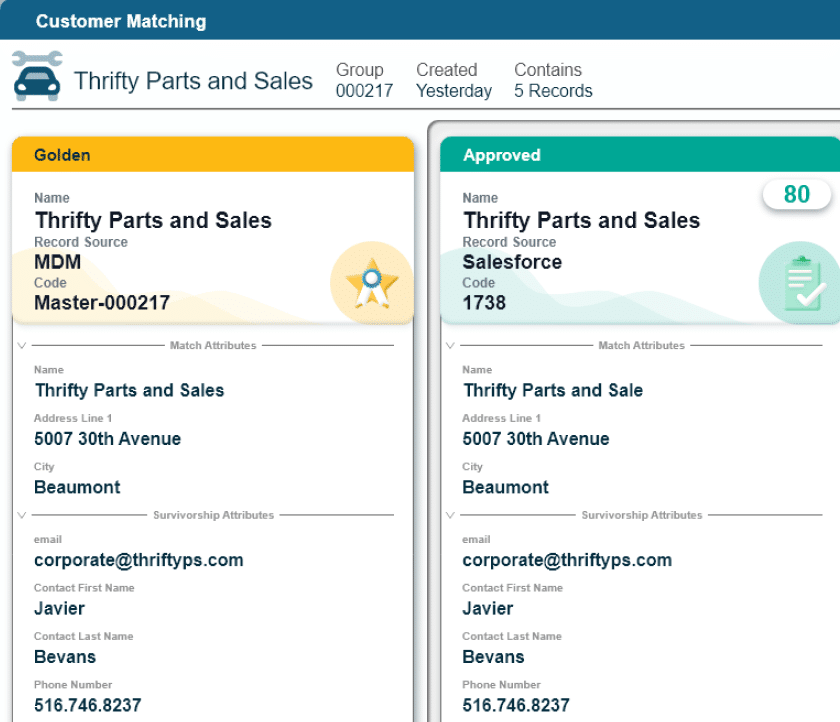
Complete & Validated PA Submission Data
- Fill In the Gaps: MDM brings advanced automation to aggregate data from multiple internal and external sources to automatically assemble comprehensive patient, plan, and diagnostic data required for PA submission.
- Identify Errors: Data quality rules can spot and highlight abnormal values, missing information and bring these to the attention of prior authorization and insurance teams, ensuring that submissions are complete and accurate the first time.
- Continuous Updating: Patient coverage changes, sometimes even during the course of care. MDM can collect and aggregate plan member data from insurers to identify changes, lapses, or secondary coverage that may not have been reported by the patient.
Accelerate Care Delivery & Reduce Costs
- Reduce Billing & Collections Costs: Even a small reduction in initially denied claims and appeals can significantly reduce billings costs estimated to be over $40 billion annually in the US. (Source)
- Accelerate Receivables: Reduce pending receivables for claims under review or appeal by getting authorization requests submitted correctly the first time.
- Delivery More Timely Care: Fewer PA submission errors and appeals allows healthcare providers to deliver necessary care faster.
- Reduce Care Downgrades: With more complete patient history, possibly spanning multiple EHR and care facilities, payer care downgrades can be avoided or contested.
- Improve Morale: Allow care teams to focus on care delivery instead of payer-related headaches.