- HEALTHCARE Use Case
Healthcare: Enable Interoperability / CMS-0057-F
How Profisee helps healthcare providers comply with interoperability requirements with consumable data
Interoperability is more than an interface.
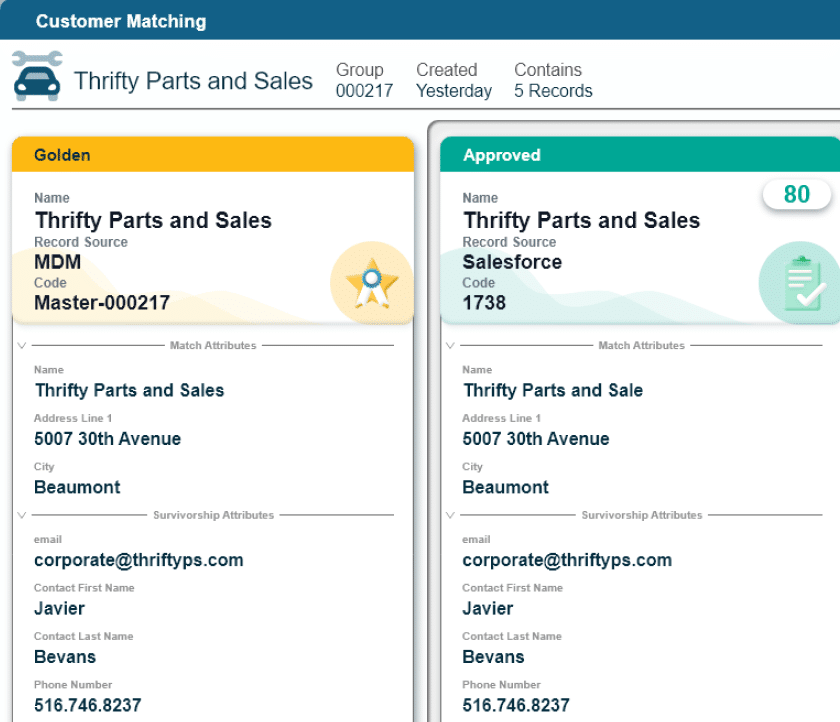
The CMS-0057-F regulations are transforming healthcare interoperability with mandates for standardized APIs, transparent data exchange, and streamlined prior authorization. To achieve compliance while maintaining operational efficiency, healthcare organizations must ensure that data exchanged across systems is accurate, complete, and validated—which is where Profisee Master Data Management (MDM) comes in.
Data Domains
Patient, Member, Plan, Reference Data
Business Problem
Manual data remediation to meet compliance
Teams Impacted
Operations, Billing, Physicians
MDM Impact
Automate data cleansing & validation, reduce costs
Incomplete, Inaccurate Data
- Incomplete Submissions: CMS submissions require data spanning multiple subject areas: patient, financial, health information, enrollment, coding and more, which can lead to missing data fields.
- Data Mismatches: Discrepancies in financial or provider data result in submission rejection, requiring investigation, remediation & resubmission.
- Invalid Codes: Coding and taxonomies for diagnosis & procedures must be complete and align, which can be challenging when data may span multiple patient visits, multiple facilities, or potentially even multiple EHRs. .
- Manual Remediation: High rejection rates lead to a substantial manual effort from clinical and finance teams to research, correct and resubmit required data, leading to excess costs, delays, and potentially compliance violations.
Deliver Compliance with Complete Data
- Fill In the Gaps: MDM brings advanced automation to aggregate data from multiple internal and external sources to automatically assemble comprehensive patient, plan, and diagnostic data required for interoperability and CMS=0057-F
- Identify Errors: Data quality rules can spot and highlight abnormal values, missing information and flag these for correction ensuring that submissions are complete and accurate the first time.
- Continuous Updating: Patient coverage changes, sometimes even during the course of care. MDM can collect and aggregate plan member data from insurers to identify changes, lapses, or secondary coverage that may not have been reported by the patient.
Reduce Costs, Improve Operational Efficiency
- Reduce Compliance Costs: Leverage powerful automation to streamline the process of assembling and validating data for CMS submissions.
- Accelerate Prior Authorizations: With complete and validated data at the ready, processing submissions can be done quickly and automatically without manual data review & remediation.
- Delivery More Timely Care: With clinical, patient, and coverage data submitted correctly the first time, initial approval rates improve allowing for faster care delivery.
- Improve Receivables: With prior authorizations completed reliably prior to care, hospitals can reduce the number of disputed claims.
- Offset Compliance Cost with Efficiencies: Without automation, CMS compliance can be costly. With MDM, costs are reduced and efficiency improved.